The latest study on myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) delves deep into the intricacies of this perplexing illness. ME/CFS, characterized by profound fatigue, especially following minimal exertion, often leaves patients struggling to find understanding and appropriate medical care.
Published in Nature Communications, the research led by Avindra Nath from the U.S. National Institute of Neurological Disorders and Stroke confirms the biological basis of ME/CFS. By examining 17 individuals with ME/CFS alongside 21 healthy controls, the study uncovers differences in brain activity, immune function, and other physiological markers.
These findings underscore the multifaceted nature of ME/CFS, as noted by Jo Cambridge, an immunologist at University College London. However, the study’s lengthy duration and extensive collaboration among over 75 scientists highlight the challenges of systematically studying ME/CFS. Despite significant investment in time and resources, advocates like Brian Vastag stress the need for further research initiatives to accelerate progress in understanding and addressing ME/CFS.
Recruiting participants posed initial obstacles, with the study focusing on individuals whose symptoms emerged post-infection. However, several participants were later diagnosed with unrelated medical conditions, revealing gaps in diagnostic practices and healthcare provision for ME/CFS patients.
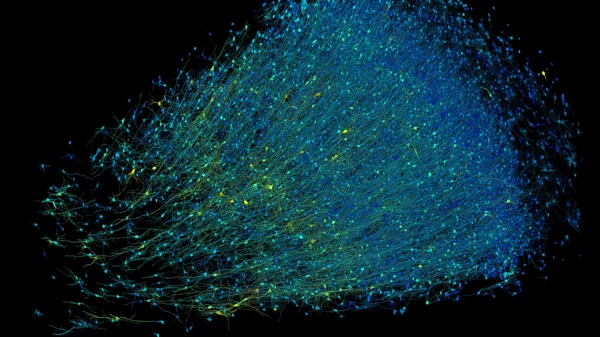
During the extensive evaluation at the National Institutes of Health (NIH), participants underwent various tests, including biopsies and imaging scans. While muscle tissue analysis showed no definitive differences, functional MRI revealed decreased brain activity in regions involved in movement control, suggesting a central role of the brain in ME/CFS pathophysiology.
Nancy Klimas from Nova Southeastern University emphasizes the brain’s involvement in ME/CFS, with abnormalities in brain signaling contributing to the debilitating fatigue experienced by patients. Despite extensive investigation, the exact mechanisms driving these abnormalities remain elusive.
Moreover, immune dysfunction and autonomic nervous system abnormalities were observed in ME/CFS patients, indicating a broader systemic involvement. Nath and his team speculate that immune dysfunction may influence brain function, opening avenues for potential therapeutic interventions.
As the research continues, the urgent need for effective treatments for ME/CFS becomes increasingly apparent. Patients, like Vastag and his late partner Beth Mazur, are counting on ongoing research efforts to provide hope and relief for those living with this debilitating condition.