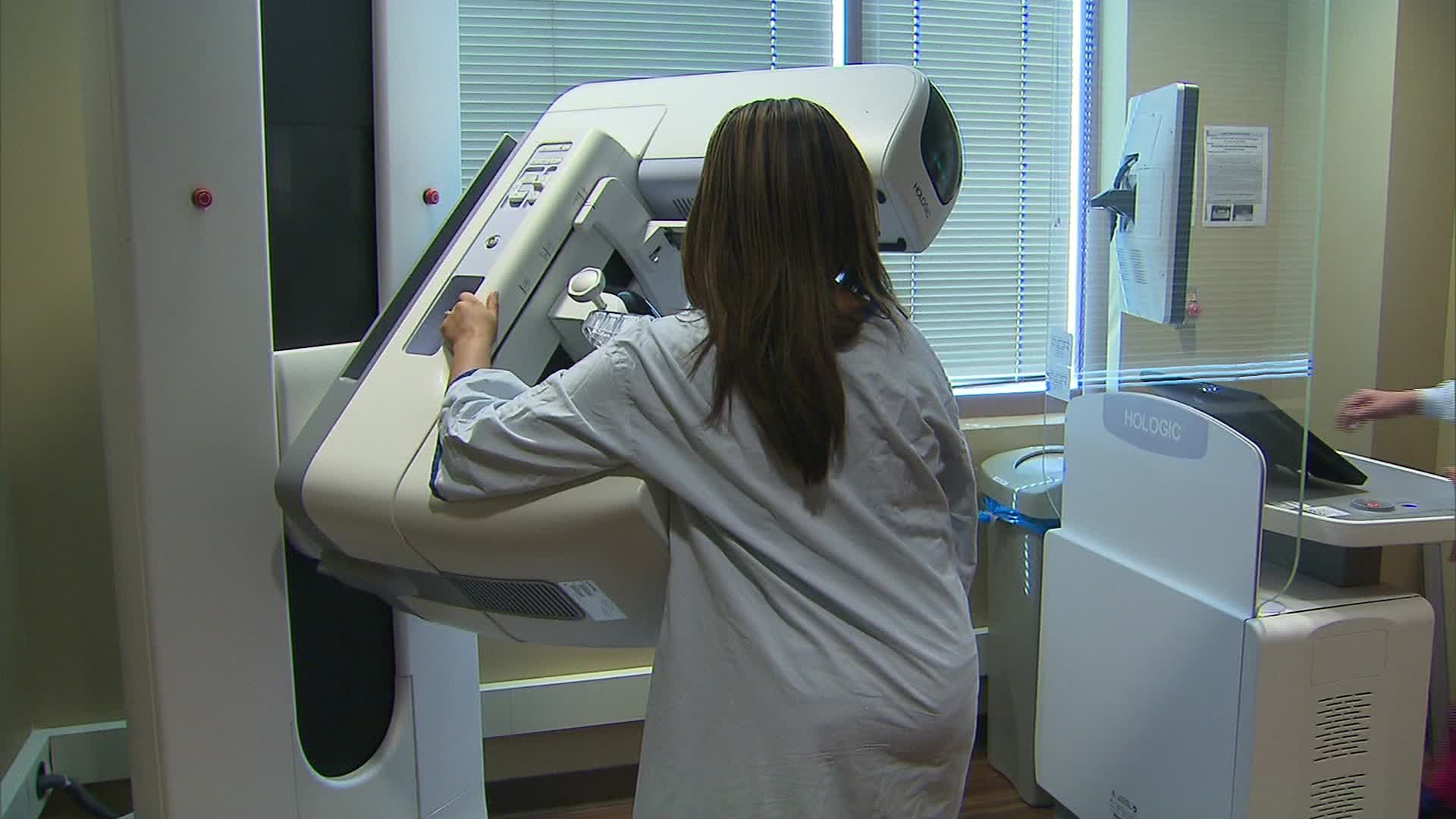
New Recommendations for Breast Cancer Screening
Introduction: Recent recommendations from the US Preventive Services Task Force (USPSTF) advise women to undergo a mammogram every other year starting at age 40 until age 74. This represents a shift from previous guidelines, which suggested biennial mammograms beginning at age 50, leaving the decision for women in their 40s to their discretion. The updated guidelines, published in JAMA, aim to enhance early detection and reduce breast cancer mortality rates.
Who’s Affected: The new recommendations apply to individuals assigned female at birth, including cisgender women, transgender men, and nonbinary people, who are at average risk of breast cancer. However, those with specific risk factors, such as a personal history of breast cancer or genetic markers like BRCA1 or BRCA2, should adhere to personalized screening plans outlined by their healthcare providers.
Benefits of Screening: Early detection through mammography plays a crucial role in reducing mortality rates associated with breast cancer, the second most common cancer among American women. By diagnosing cases at an early stage, before cancer spreads, the risk of death from the disease is significantly lowered.
Why Biennial Instead of Annual Screening?: While some critics argue for annual screenings, the USPSTF defends its biennial recommendation, citing evidence that it maintains efficiency while reducing false positives compared to annual screenings. Dr. Wendie Berg of the University of Pittsburgh School of Medicine suggests that annual screenings may offer greater overall benefits, especially for premenopausal women and those from minority racial and ethnic groups.
Addressing Concerns: Some concerns have been raised regarding the USPSTF’s blanket recommendations for individuals with different risk profiles. Organizations like Susan G. Komen emphasize the importance of personalized screening plans based on factors such as family history and breast density. This individualized approach ensures appropriate screening frequency and type for each person.
Access and Utilization: There are fears that the updated recommendations might lead to decreased access and utilization of screening services, potentially resulting in more late-stage diagnoses. While the guidelines are tied to health plans covering screening costs, the emphasis on biennial screening may deter individuals from seeking annual screenings, raising concerns about delayed diagnoses and increased healthcare costs.
Conclusion: In summary, the USPSTF’s updated recommendations aim to improve breast cancer screening practices, emphasizing biennial mammograms starting at age 40. While the guidelines provide a valuable framework, individuals are encouraged to engage in discussions with their healthcare providers to determine the most suitable screening approach based on their unique risk factors and medical history.