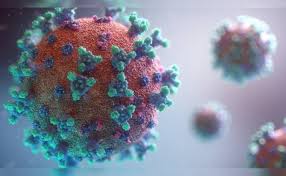
It’s crucial to acknowledge that while much of the country and our government might feel like we’ve put the worst of the pandemic behind us, the reality is that COVID-19 isn’t going anywhere. Recent developments with the emergence of new variants, sometimes referred to as “FLiRT” variants, serve as a stark reminder of this fact and the ongoing challenges some individuals continue to face.
Despite the hopeful news that weekly hospitalizations are at their lowest since the pandemic’s onset, there’s a concerning shift in reporting procedures. As of May 1st, hospitals are no longer obligated to provide COVID-19-related data to the federal government. This change comes at a time when the dominant variant, KP.2, now represents nearly a quarter of all infections, surpassing its predecessor, JN.1.
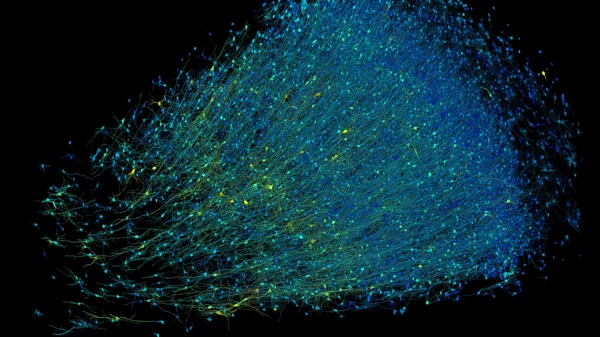
These FLiRT variants, including KP.2 and its counterparts like KP.1.1, are named for their specific mutations. While they are descendants of the omicron strain, they boast spike protein mutations that enhance their transmissibility. However, according to experts like William Schaffner from Vanderbilt University School of Medicine, there’s no substantial difference in the severity of illness caused by these variants compared to earlier strains.
Although the spike protein mutations may potentially reduce the efficacy of vaccines and natural immunity against these variants, lab tests indicate that they still offer significant protection against severe disease. Essentially, we’re now navigating through what Schaffner describes as the “omicron era,” where COVID-19 is becoming a part of our seasonal health landscape. It’s a reminder that this virus is now endemic, and we must adapt to manage it as part of our routine health practices.