A heartbreaking situation has unfolded for newborn twins diagnosed with a rare, often fatal genetic disorder, as their family’s insurance company has denied coverage for life-saving treatment. Eli and Easton Reed, born on March 31, 2024, were diagnosed with spinal muscular atrophy shortly after their arrival.
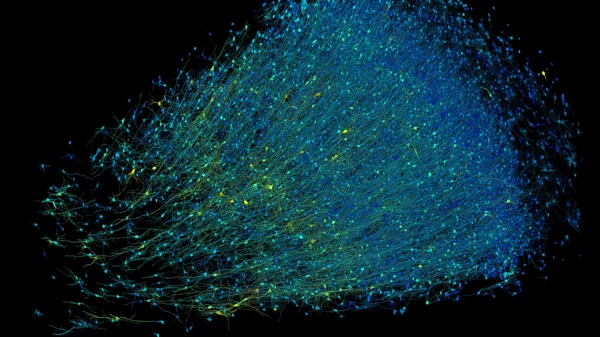
Spinal muscular atrophy is a condition that affects specialized nerve cells in the brain and spinal cord, leading to potentially severe consequences. While there is currently no cure, managing symptoms and preventing complications are key components of treatment.
For the Reed family in St. Joseph, Missouri, the recommended treatment for the twins included the medication Zolgensma. However, their insurance company abruptly stopped covering the medication just one day before the twins were born, leaving the family in a devastating predicament.
Time is crucial in administering treatment, as the twins currently show no symptoms. Their mother, Amanda Reed, emphasized the urgency, stating that once symptoms manifest, they become irreversible. However, despite their efforts to explore all options, the cost of Zolgensma is staggering, ranging from $1 million to $2.5 million per child.
Zolgensma is described as a one-time treatment that targets the genetic root cause of spinal muscular atrophy, halting the disease’s progression. Despite appeals and an emergency meeting with the insurance company, the family’s plea for coverage was denied on April 26, leaving them responsible for the daunting expense.
Facing the possibility of life or death decisions beyond their control, the twins’ father, Austin Reed, expressed profound anguish. Without treatment, the twins’ prognosis is dire, with a grim outlook for infants with type 1 spinal muscular atrophy.
The Reed family’s plight serves as a stark reminder of the challenges families face in navigating healthcare systems and the profound impact of insurance decisions on individual lives.