In a groundbreaking development, scientists from Stanford University believe they have unraveled a critical aspect behind the disproportionately higher rates of autoimmune diseases in women. Their research, published in the journal Cell, identifies a molecule called Xist as a potential driver of female-biased autoimmunity. According to Howard Chang, PhD, the senior author of the study and a professor of dermatology and genetics at Stanford, the study reveals that a specific RNA known as Xist, produced exclusively in female cells, could be a major contributor to autoimmunity. This discovery opens up new possibilities for the diagnosis and treatment of autoimmune diseases, which affect approximately 50 million people in the United States, with up to 80% of them being women.
The study delves into the longstanding mystery surrounding the prevalence of autoimmune diseases in women, attributing it to a single, female-specific RNA. This RNA, Xist, plays a pivotal role in regulating immune responses. The ratio of females to males in autoimmune diseases like lupus and Sjorgen’s syndrome is disproportionately high, with figures reaching 9 to 1 and even 19 to 1, respectively. Researchers at Stanford have zeroed in on the fundamental differences between the biological sexes, emphasizing the role of X chromosomes.
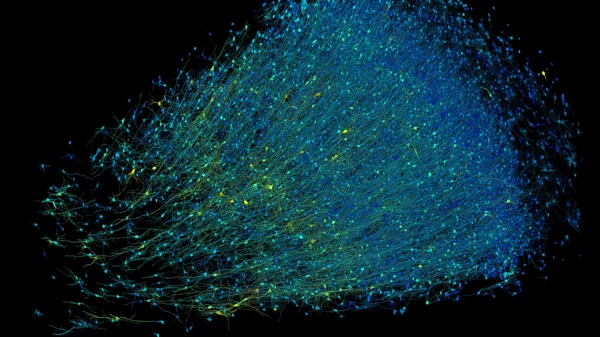
Biologically, females possess two X chromosomes, while males have one X and one Y chromosome. The risk of overproducing proteins due to the presence of two X chromosomes is addressed by a process called X-chromosome inactivation, facilitated by the Xist molecule. This process results in unique combinations of RNA, DNA, and protein complexes, triggering a robust immune response in females.
The study conducted experiments on mice with lupus, demonstrating that an increase in Xist significantly intensified the severity of the disease. The researchers also found autoantibodies to protein complexes associated with Xist in blood samples from over 100 people with autoimmune diseases. Importantly, the research challenges the conventional approach of using male cell lines as a reference, overlooking critical components in female patients that contribute to autoimmune susceptibility.
Dr. Daniel Arkfeld, a rheumatologist with Keck Medicine of USC in California, hails the Stanford study as a pivotal advancement in autoimmune disease research. He considers it a potential game-changer in understanding and eventually intervening in the mysteries of autoimmune disorders. This breakthrough could pave the way for innovative treatments, potentially involving gene manipulation to target chromosomal expressions.
Despite the progress, autoimmune diseases remain enigmatic, and researchers globally are grappling with unanswered questions. While treatments exist for some diseases, the challenge lies in prevention. Researchers like Ranjeny Thomas from The University of Queensland emphasize the need to explore preventive measures, monitoring populations before the onset of diseases and investigating immunotherapy interventions. The study sheds light on the intricate mechanisms underlying autoimmune diseases, offering hope for future breakthroughs in prevention and treatment strategies.