Advances in medicine have brought us to a remarkable juncture where we can directly alter human genetics, offering the potential to tackle diseases by tweaking troublesome DNA strands. At the forefront of this revolution is CRISPR, the groundbreaking gene-editing technology that earned its creators the Nobel Prize in Chemistry back in 2020.
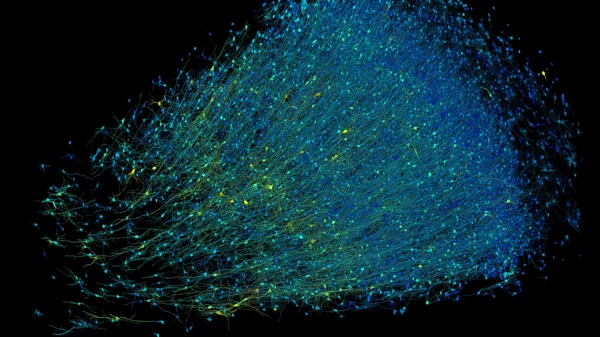
CRISPR has revolutionized medical research over the past decade by leveraging bacterial proteins to target disease-causing genes. Unlike previous gene-editing methods, CRISPR enables faster, cheaper, and more precise genome editing, giving scientists unprecedented control over gene insertion and activation.
The recent approval of the first CRISPR-based therapy, Casgevy, by the US FDA and the European Commission marks a significant milestone in medicine. Designed to treat sickle cell disease, Casgevy exemplifies the potential of CRISPR to revolutionize treatments by modifying or replacing problematic genes.
However, realizing CRISPR’s full potential hinges on addressing a crucial obstacle: the lack of diversity in genetics research. Biases in genetic databases and biobanks could exclude certain communities from benefiting from CRISPR innovations fully.
Closing this gap is essential for developing effective gene therapies. Genetic data have already transformed cancer research, guiding drug design and patient treatment. By understanding the genetic basis of diseases, such as cancer, researchers can tailor treatments to target specific mutations.
CRISPR, derived from a bacterial immune system, functions as a molecular tool for editing genes. By adapting bacterial CRISPR components to target human DNA, scientists can precisely edit problematic genes associated with diseases.
The breakthrough sickle cell treatment exemplifies CRISPR’s therapeutic potential. Sickle cell disease, caused by a mutation in a single gene, presents an ideal target for gene therapy. Casgevy targets the BCL11A gene, which regulates hemoglobin production. By inactivating this gene, Casgevy promotes the production of normal hemoglobin, alleviating the symptoms of sickle cell disease.
Initial trials of Casgevy have shown promising results, with patients experiencing relief from severe pain crises. However, the effectiveness of gene therapies may vary based on individual genetic diversity. Therefore, it’s crucial to ensure that genetic research reflects the diversity of the patient population to maximize the benefits of CRISPR-based therapies for all individuals.